초록접수 현황
| 17F-226 | 구연 미채택시 English competition forum 발표 |
Fate of Malperfused Kidney in Acute DeBakey Type I Aortic Dissection
Shin-Young Lee¹, Woon Heo¹, Suk-Won Song¹, Tae-Hoon Kim¹, Min-Young Baek¹, Kyung-Jong Yoo², Bum-Koo Cho³
¹Department of Thoracic and Cardiovascular Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea., ²Department of Thoracic and Cardiovascular Surgery, Severance Hospital, Yonsei University College of Medicine, The Korea Heart Foundation, Seoul, Republic of Korea., ³The Korea Heart Foundation, Seoul, Republic of Korea
Purpose : To review the perioperative and postoperative functional changes in malperfused kidney in acute DeBakey type I aortic dissection.
Methods : Of 191 patients, who underwent emergency repair for acute type I aortic dissection from 2010 to 2015, 141 patients were reviewed and grouped as malperfusion (n=37) and normal (n=104). All computed tomographic scan result, serum creatinine, urea nitrogen and estimated glomerular filtration values at preoperative, postoperative, discharge, first outpatient clinic visit, and latest follow-up were collected.
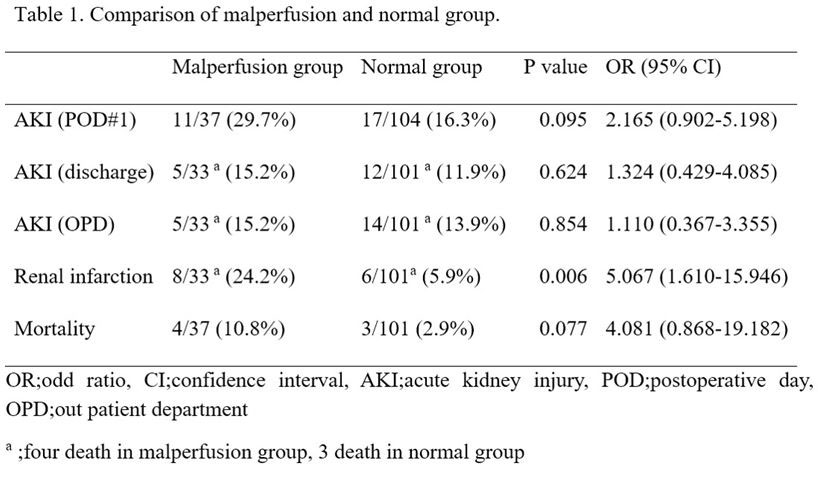
Results : There was no difference between normal and malperfusion group in total cardiopulmonary bypass time (151.4±39.2 vs. 156.1±69.8, p=0.696) and total operation time (276.0±72.7 vs. 270.4±74.6, p=0.691). The incidence of renal infarction were higher in malperfusion group (24.2% vs. 5.9%, p=0.006). However, there were no differences in BUN (16.0±10.2 vs. 19.6±16.1, p=0.232), serum creatinine (0.8±0.3 vs. 0.9±0.5, p=0.156) and eGFR (91.8 ±17.4 vs. 84.5 ±22.3, p=0.054) between the malperfusion and normal groups at first outpatient clinic visit. The incidence of acute kidney injury, where the serum creatinine was increased 1.5 times the baseline value, in both groups showed no difference at first outpatient clinic follow-up between the normal and malperfusion groups(13.9% vs. 15.2%, p=0.854). The in-hospital mortality was 4.96 %( total 7 out of 141 patients) with 4 patients in malperfusion group (10.8%, p=0.077) and 3 in normal group (2.9%, p=0.077).
Conclusion : There were no difference in in-hospital mortality and long-term renal function between the two groups. With prompt established reperfusion, renal malperfusion is not the risk factor for AKI and increased mortality.
Methods : Of 191 patients, who underwent emergency repair for acute type I aortic dissection from 2010 to 2015, 141 patients were reviewed and grouped as malperfusion (n=37) and normal (n=104). All computed tomographic scan result, serum creatinine, urea nitrogen and estimated glomerular filtration values at preoperative, postoperative, discharge, first outpatient clinic visit, and latest follow-up were collected.
Results : There was no difference between normal and malperfusion group in total cardiopulmonary bypass time (151.4±39.2 vs. 156.1±69.8, p=0.696) and total operation time (276.0±72.7 vs. 270.4±74.6, p=0.691). The incidence of renal infarction were higher in malperfusion group (24.2% vs. 5.9%, p=0.006). However, there were no differences in BUN (16.0±10.2 vs. 19.6±16.1, p=0.232), serum creatinine (0.8±0.3 vs. 0.9±0.5, p=0.156) and eGFR (91.8 ±17.4 vs. 84.5 ±22.3, p=0.054) between the malperfusion and normal groups at first outpatient clinic visit. The incidence of acute kidney injury, where the serum creatinine was increased 1.5 times the baseline value, in both groups showed no difference at first outpatient clinic follow-up between the normal and malperfusion groups(13.9% vs. 15.2%, p=0.854). The in-hospital mortality was 4.96 %( total 7 out of 141 patients) with 4 patients in malperfusion group (10.8%, p=0.077) and 3 in normal group (2.9%, p=0.077).
Conclusion : There were no difference in in-hospital mortality and long-term renal function between the two groups. With prompt established reperfusion, renal malperfusion is not the risk factor for AKI and increased mortality.
책임저자: Suk-Won Song
Department of Thoracic and Cardiovascular Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
발표자: Shin-Young Lee, E-mail : yonseimed@gmail.com