초록접수 현황
| 17F-005 | English competition forum |
Short Inverted Graft Anastomosis for Proximal Aortic Repair in Acute Type A Aortic Dissection: Technique and Surgical Experiences
Seung Ri Kang, Joon Bum Kim
Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, Ulsan University College of Medicine, Seoul, Republic of Korea
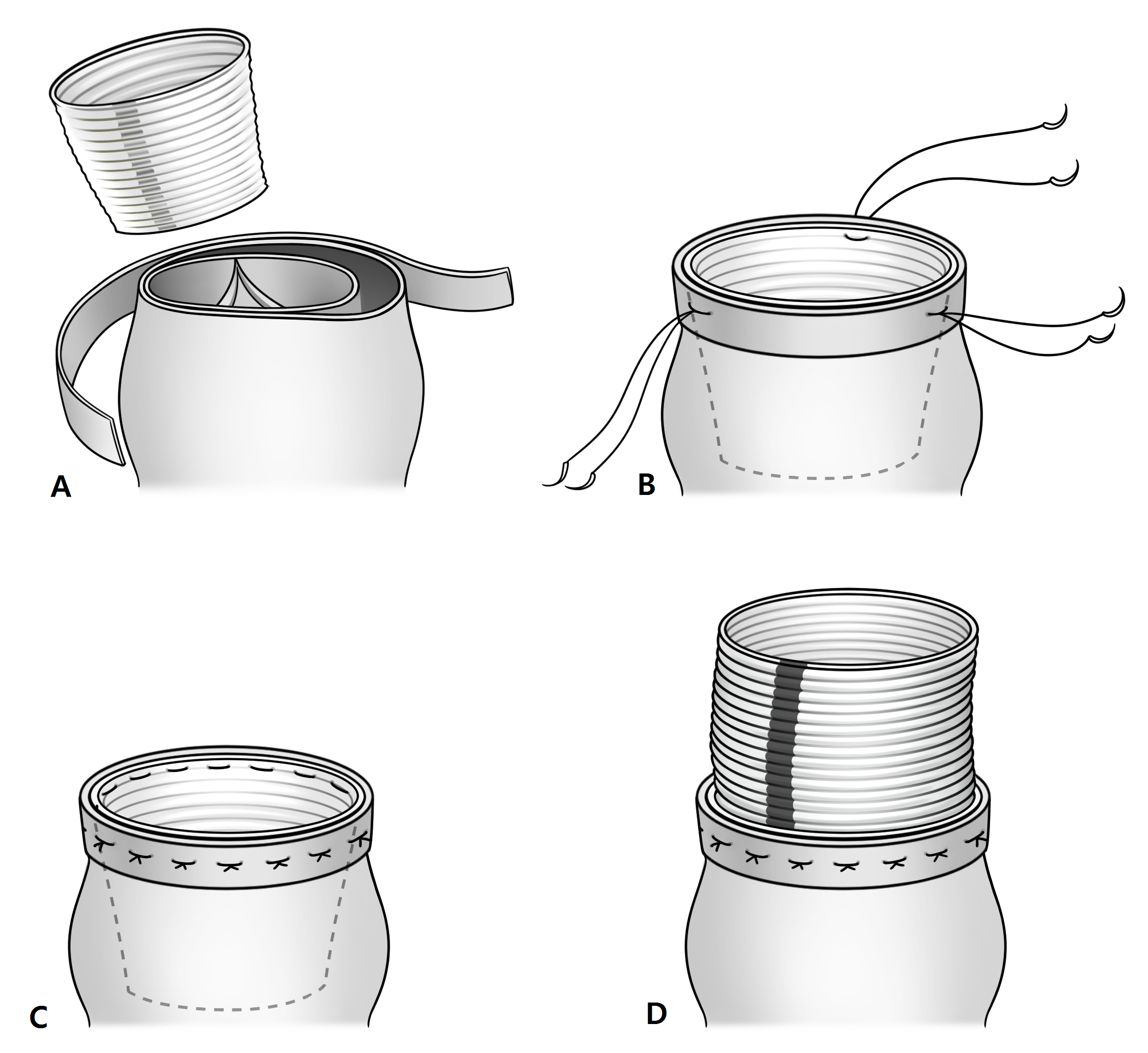
Purpose : Aortic surgery in the setting of an acute aortic dissection (AD) is a challenging task carrying high risks of anastomosis sites bleeding. In order to efficiently minimize bleeding in the proximal aorta during open repair of ascending aorta, a technique of using inversion of an artificial graft for proximal anastomosis has been utilized.
Methods : From November 2015 through June 2017, a total of 19 patients undergoing ascending aorta repair using the inverted graft anastomosis were reviewed. The proximal repair was conducted during hypothermic induction under mid-ascending aortic clamping in all patients.
Results : Majority (15/19, 78.9%) of the patients underwent surgery due to acute aortic dissection (AD), and the remaining (4/19, 21.1%) due to ascending aortic aneurysm. Total arch (N=2) or hemiarch (N=13) replacements were combined in 18 patients (83.3%). Upper partial sternotomy was used in 2 patients (10.5%). The median cardiopulmonary bypass , aorta cross clamp, and total circulatory arrest times were 79 minutes (range 56-182), 64 minutes (range 49-95) and 7 minutes (range 4-31), respectively. The median time from incision to wound closure was 193 minutes (range 114-312). There was no case of mortality, low cardiac output syndrome, postoperative bleeding, or neurologic deficit. However, 3 patients (15.8%) showed major complications: mediastinitis in 1, coronary insufficiency requiring additional right coronary bypassing in 1 and root pseudo-aneurysm requiring re-exploration for complete root replacement in 1.
Conclusion : The short inverted graft anastomosis technique for proximal aortic repair may be a reasonable option in terms of Time-efficiency and excellent hemostasis in well selected patients.
Methods : From November 2015 through June 2017, a total of 19 patients undergoing ascending aorta repair using the inverted graft anastomosis were reviewed. The proximal repair was conducted during hypothermic induction under mid-ascending aortic clamping in all patients.
Results : Majority (15/19, 78.9%) of the patients underwent surgery due to acute aortic dissection (AD), and the remaining (4/19, 21.1%) due to ascending aortic aneurysm. Total arch (N=2) or hemiarch (N=13) replacements were combined in 18 patients (83.3%). Upper partial sternotomy was used in 2 patients (10.5%). The median cardiopulmonary bypass , aorta cross clamp, and total circulatory arrest times were 79 minutes (range 56-182), 64 minutes (range 49-95) and 7 minutes (range 4-31), respectively. The median time from incision to wound closure was 193 minutes (range 114-312). There was no case of mortality, low cardiac output syndrome, postoperative bleeding, or neurologic deficit. However, 3 patients (15.8%) showed major complications: mediastinitis in 1, coronary insufficiency requiring additional right coronary bypassing in 1 and root pseudo-aneurysm requiring re-exploration for complete root replacement in 1.
Conclusion : The short inverted graft anastomosis technique for proximal aortic repair may be a reasonable option in terms of Time-efficiency and excellent hemostasis in well selected patients.
책임저자: Joon Bum Kim
Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, Ulsan University College of Medicine, Seoul, Republic of Korea
발표자: Seung Ri Kang, E-mail : medparme@gmail.com